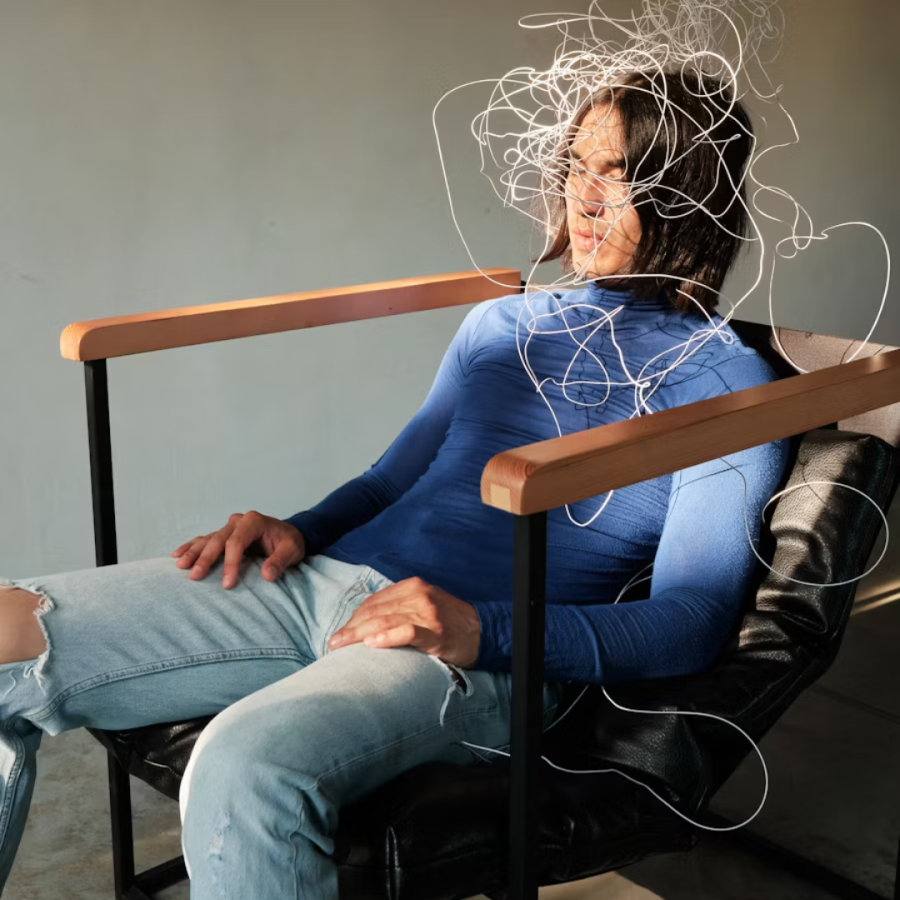
After my second child was born, I began experiencing disturbing, intrusive images: vivid scenes of dropping her as I climbed the stairs, or her stroller breaking free and rolling into traffic. The thoughts felt so real that my body would flood with panic. I didn’t know what to do with the terror these images brought, so I developed strategies: I walked impossibly slowly up the stairs, gripping her so tightly my arms ached. I gripped the stroller when we were on walks, avoiding hills as much as possible, even when it added 30 minutes to our walk.
At the time, I was in therapy for depression and anxiety, but when I tried to explain these thoughts to my therapist, neither of us knew what to make of them. Were they just normal new parent worries taken a bit too far? Part of postpartum anxiety? Something else entirely? Without a framework to understand what I was experiencing, I continued to struggle, working harder and harder to keep the images at bay, not realizing that my coping strategies were actually feeding the cycle.
It wasn’t until much later that I recognized what I had experienced: intrusive thoughts triggering intense anxiety, followed by compulsive behaviors designed to neutralize the fear: the classic OCD feedback loop. Looking back, I often wonder if I would have met the diagnostic criteria during that period, or if I came close. What I do imagine is that proper recognition could have changed everything. I could have received more effective treatment instead of struggling alone with my fears.
I share this not to self-diagnose retrospectively, but to illustrate how easily OCD symptoms can be misunderstood, even by mental health professionals. My experience raises important questions about recognition and diagnosis: When do intrusive thoughts cross the line into OCD? How do we distinguish OCD from other anxiety disorders or from normal postpartum worries? And what makes the difference between having some OCD-like symptoms and meeting the full diagnostic criteria?
OCD is a complex diagnosis, and while it’s not uncommon, it is still often misdiagnosed and missed by skilled clinicians. Because of this, individuals who are experiencing symptoms of OCD don’t receive the support they need, and continue to suffer needlessly.
What is OCD? What is OCD not? What myths about OCD are most common?
Obsessive–Compulsive Disorder is a mental health condition marked by obsessions and compulsions. Obsessions are unwanted, intrusive thoughts, images, or urges that spark anxiety, disgust, doubt, or a sense that something is not right. Compulsions are anything a person does, either outwardly or in their mind, to get relief from the discomfort the obsession brings.
Obsessions can center on a wide range of themes: contamination, health, safety, sexual or religious worries, morality, identity, relationship doubts, symmetry, or the need for things to feel “just right.” We will get into more specifics later in this article.
OCD is a disorder that takes up a lot of time and life. Clinically, it takes an hour or more out of someone’s day. In fact, when OCD is severe, intrusive thoughts and compulsions can surface every few minutes. And yet, many people with OCD, even those with severe cases, find ways to work around their struggles. People become experts at masking or concealing their symptoms and may be highly productive or appear “high functioning”. Still, behind the scenes, OCD can make it hard to feel fully present or live a fulfilling life.
One important aspect of OCD is the anxiety that accompanies it. In fact, OCD was once classified as an anxiety disorder until the release of the DSM-5 in 2013. While not all experts agree that this was the correct decision, there is a consensus that OCD is characterized by anxiety, which is brought on by intrusive thoughts.
The following are some common myths we can retire about OCD:
It’s important to understand that OCD isn’t a personality quirk. Although many people still don’t understand that OCD is a serious disorder, research explains that OCD is a clinical syndrome characterized by measurable impairment, rather than a simple preference for neatness or order. While the symptoms of OCD exist on a spectrum (like many other mental health diagnoses), and you can have some of the symptoms without meeting the full diagnostic criteria, saying things like “I’m a little OCD” makes it tougher for people who actually have OCD to spot real symptoms and reach out for help. It can also mean diagnoses get missed or delayed, especially when symptoms are invisible or feel taboo to share.
People with OCD aren’t choosing their obsessions or compulsions. Sheer willpower cannot treat OCD.
Insight isn’t all-or-nothing. Most people with OCD are self-aware and recognize that their intrusive thoughts are irrational. Even when someone knows a fear is unlikely, the urge to reduce distress still takes over. Writer David Sedaris has described how as a child, if he lost count of his steps walking home from school, he felt compelled to return to school and start over—even though he knew it made no logical sense. That tension is quintessential OCD and explains why effective care addresses both overt and covert rituals rather than debating the thought content.
What OCD is not: Understanding the boundaries
OCD exists on a continuum, but not everyone with intrusive thoughts has OCD. Lots of people experience unwanted thoughts or like things organized in certain ways. And OCD can overlap with other conditions, which makes things even more confusing.
Intrusive thoughts about harm can occur in postpartum anxiety or depression. Perfectionism can be part of generalized anxiety. Health worries can be part of illness anxiety disorder. What distinguishes OCD is the specific obsession-compulsion cycle and the way compulsions temporarily relieve but ultimately perpetuate the anxiety.
The key distinctions are:
Time and impairment: Does it consume more than an hour per day? Does it significantly interfere with work, relationships, or daily functioning?
The compulsive response: It’s generally not just having the thought, but the thought is often connected to feeling driven to perform rituals to reduce the anxiety.
The feedback loop: Does attempting to neutralize the thought actually reinforce it and make it stronger?
So what is the feedback loop? It’s one of the most misunderstood aspects of OCD and a big part of what perpetuates the disorder. This cycle begins when a person experiences a distressing and intrusive thought or image, triggering intense stress and anxiety. To alleviate this discomfort, the person feels compelled to engage in specific rituals or actions. Over time, their brain begins to associate this compulsion with a sense of relief, even if performing it is time-consuming or painful. This connection reinforces the behavior, creating a feedback loop that intensifies the cycle.
As this pattern continues, the relief provided by the compulsion gradually diminishes, leading the person to increase the frequency or intensity of the ritual in search of relief. Through this loop, OCD begins to increasingly consume a person’s life, as they find themselves investing more effort to obtain even a brief moment of relief from their anxiety.
OCD vs. OCPD: A critical distinction
People often confuse OCD with Obsessive-Compulsive Personality Disorder (OCPD), but they’re quite different:
OCD involves unwanted, distressing intrusive thoughts (obsessions) and behaviors performed to reduce anxiety (compulsions). People with OCD typically recognize their thoughts are irrational and want relief from them.
OCPD is also a diagnosis in the DSM-5. It’s a personality disorder characterized by a pervasive pattern of preoccupation with orderliness, perfectionism, and control. People with OCPD generally see their way of doing things as correct and don’t experience their behaviors as intrusive or distressing, meaning that they’re ego-syntonic, or consistent with their sense of self. For example: Someone with OCD might compulsively check that items are aligned because they fear something bad will happen if they don’t. Someone with OCPD believes things should be organized in a specific way and may become frustrated when others don’t follow their standards.
What are common signs and themes of OCD? And what are some less commonly known themes?
Compulsions show up in two forms. Overt compulsions are visible and easily observable behaviors, such as re-washing hands, double-checking locks or appliances, re-reading or rewriting text, arranging items until they feel “just right,” repeating specific actions, or seeking reassurance from others. These physical compulsions are often easier to identify and are what we usually associate with OCD compulsions.
Covert compulsions are subtler, mental maneuvers that are harder to spot. These may include activities like mental reviewing, counting, trying to analyze or “figure things out,” rehearsing conversations in one’s mind, silently repeating words or prayers, self-reassurance, scanning one’s body for specific sensations, or seeking certainty through excessive online research. Additionally, people may seek reassurance indirectly by comparing themselves to others or observing their reactions. And avoidance behaviors, like steering clear of certain situations, objects, topics, or sensations, can also serve as compulsions.
Common OCD themes include fears of contamination and illness, anxieties surrounding harm and responsibility (such as worries about fires, safe driving, or the potential consequences of leaving dangers unaddressed), and a preoccupation with achieving perfection or symmetry, where something feels “off” rather than outright dangerous.
Just as common, but less visible to outsiders, are taboo or disturbing intrusive thoughts that may involve violent or sexual content, doubts related to identity or orientation, uncertainties in relationships, and health-related obsessions, like hyper-awareness of breathing, heartbeat, or swallowing. Other themes include existential questioning about the meaning of life or reality, doubts about memories and “real events” often requiring exhaustive timeline reconstruction, perinatal and parenting anxieties, as well as superstitions involving “magical” rules about numbers, words, or rituals.
These themes can overlap and may shift over time, yet the underlying cycle of obsession and compulsion remains constant, perpetuating the challenges faced by those living with OCD.
What about “Pure O” OCD?
Many people say, “I only have thoughts,” because their rituals are internal. Some may genuinely experience primarily obsessional OCD without significant compulsions, and this can still be incredibly distressing and interfere with daily life. However, clinical research and newer reviews suggest that what is often labeled as “Pure O” typically includes covert compulsions that can be easily overlooked. These include things like mental repetition, reviewing, self-reassurance, confession, online checking, or subtle avoidance strategies. These responses are easy to miss, but they still maintain the symptoms, even when they’re not obvious to others or to the person experiencing them.
When mental rituals and covert reassurance are counted, many people who thought they only had obsessions recognize they’ve been engaging in compulsive responses all along. Examples of these hidden patterns include compulsively rewriting or deleting posts and emails, repeatedly taking screenshots or checking accounts “just to be sure,” engaging in mental counting, and replaying commutes or conversations in search of certainty. While these actions can seem ordinary, they too function as compulsions that feed into the OCD loop.
Whether someone has purely obsessional OCD or obsessions with subtle mental compulsions, the suffering is real and the need for proper support remains the same. If intrusive thoughts are causing significant distress or taking up substantial time in your day, it’s worth seeking help, regardless of whether you can identify clear compulsive behaviors.
What approaches are effective for treating OCD, and which aren’t?
Evidence consistently shows that Exposure and Response Prevention (ERP), a specialized form of cognitive behavioral therapy, is the gold standard for OCD treatment. ERP yields reliable results, with about 60-70% of those who commit to treatment experiencing significant improvement. While medication can help reduce symptoms for many, combining it with therapy supports more consistent progress. In very severe, treatment-resistant cases, deep brain stimulation has also shown benefits, though it is reserved for select cases.
Conversely, reassurance, open-ended talk therapy, and attempts to reason with intrusive thoughts can inadvertently sustain the OCD cycle. These methods may function as forms of neutralizing anxiety rather than affecting real change. While relaxation techniques can help reduce overall stress, they do not interrupt the OCD loop on their own. Efforts to outthink intrusive thoughts, replace them with “better” ones, or engage in excessive online research can mask compulsions and ultimately perpetuate the cycle.
What is Exposure and Response Prevention (ERP), and how does it work?
Exposure and Response Prevention (ERP) is a behavioral therapy treatment for OCD that involves intentionally exposing patients to their feared thoughts, images, sensations, or situations while consciously resisting the urge to engage in compulsive behaviors. OCD can be thought of as a disorder of ingrained habits, and untangling these habits requires time, consistent practice, and a willingness to experience discomfort while developing new responses. As Dr. Penzel notes, “You can’t fight OCD with logic, because OCD isn’t logical. It’s emotional.” ERP acknowledges this emotional reality, helping those with OCD to feel the fear, avoid the ritual, and allow their bodies to recalibrate.
In ERP, exposure involves planned and measured contact with feared stimuli, whether external cues or internal thoughts. Response prevention means deliberately choosing not to engage in rituals. As anxiety increases and eventually decreases, this decline reflects the brain’s adaptation to the trigger. With repetition, the nervous system learns to stop perceiving the trigger as an urgent threat. Clinicians monitor distress, provide support through the anxious peak, and do not leave until the discomfort subsides without resorting to compulsions. The skill lies not in fighting thoughts but in allowing them to exist and realizing you can handle the discomfort. In this way, the relief experienced comes from retraining the mind.
ERP is adaptable to various themes. For instance, someone with sensorimotor OCD might intentionally focus on their breathing or blinking, while a person with moral scrupulosity could write and read a feared sentence without engaging in debates or seeking reassurance.
Some people find it helpful to combine ERP with other approaches. Medication can provide support, particularly in the beginning stages of treatment. Cognitive techniques that address distorted beliefs, especially where people believe that thinking something makes it more likely to happen, can also be useful alongside ERP. The key is that these additions support rather than replace the core work of exposure and response prevention
How can loved ones support without feeding compulsions?
Families and partners can play a crucial role in supporting someone undergoing OCD treatment by avoiding the reinforcement of compulsions. Here are some constructive strategies:
Use clear language and set boundaries. It’s important to communicate clearly and establish predictable boundaries around behaviors. Agree on specific rules for checks, reviews, and “just to be sure” requests, and ensure you are consistent in following them.
Rethink responses to intrusive thoughts ahead of time. Instead of offering personal reassurance, loved ones can provide supportive statements that reinforce coping skills. For example, saying, “I know this is your OCD, and I believe you can let this feeling rise and fall without using a ritual,” helps encourage positive habituation.
Identify rituals and compulsions. Make note of subtler compulsive behaviors that may appear reasonable but serve the same purpose as more overt rituals. Questions like, “Did I offend them?” or requests to double-check messages can act as compulsions. Recognizing these patterns allows loved ones to step out of the reassurance cycle and support response prevention instead.
Create a support plan. If you live with someone who has OCD, consider writing a brief card that outlines what strategies are helpful and what might reinforce compulsive behavior. Practicing these responses together can prepare both parties for real-life situations, so you don’t have to improvise in difficult moments.
Keep treatment central. Remember that ERP (Exposure and Response Prevention) is a structured and effective approach to managing OCD. The goal on the toughest of days is not to eliminate distress but to help this person to remember what alleviates symptoms long-term: accepting the intrusive thought, resisting the compulsion, and allowing feelings to come and go.
How does recognizing OCD lower stigma and increase help-seeking?
Demystifying and educating ourselves about OCD is the first step in lowering stigma. When the condition is framed as a medical issue characterized by obsessions and compulsions rather than a personality trait, people start to recognize symptoms that can be treated.
Recognition also highlights the “invisible” aspects of OCD, since, as discussed, many people struggling with OCD initially dismiss their experiences as “only thoughts.” By identifying these patterns, they become more motivated to pursue appropriate treatment rather than rely on self-soothing strategies that don’t address the underlying cycle.
This understanding creates a direct pathway to evidence-based support, leading to earlier referrals, better-aligned treatments, and a greater likelihood that people remain in care long enough to achieve meaningful improvement.
What can you do if you think you have OCD?
If you’re recognizing yourself in these descriptions, here are some steps you can take:
Seek professional assessment. Given the complexity of OCD and how it overlaps with other conditions, getting an accurate diagnosis is the necessary first step. Look for a therapist who specializes in OCD or anxiety disorders and has specific training in ERP. Not all therapists are trained in treating OCD, and working with someone who understands the condition makes a real difference.
Start noticing the patterns without judgment. Begin paying attention to what triggers your intrusive thoughts and what compulsions follow. You might keep a simple log: What was the thought? What did I feel? What did I do in response? This isn’t about stopping the compulsions yet, but about building awareness of your specific OCD cycle (and this awareness matters). Understanding your patterns will be essential when you start treatment.
Resist the urge to research your way out. It is really tempting to read everything you can find about OCD, to take online assessments, or to compare your symptoms to others. But excessive researching and reassurance-seeking can actually become compulsions themselves. It can be more useful to gather enough information to seek help, and then work with a professional rather than trying to diagnose or treat yourself through the internet.
Be patient with yourself. Recovery from OCD isn’t about never having intrusive thoughts again; it’s about changing your relationship to them. The goal is to let the thoughts be there without feeling compelled to do something about them. This takes practice, and progress isn’t always linear. Some days will be harder than others, and that’s part of the process.
Know that help works. ERP has strong evidence behind it. While the idea of facing your fears without performing compulsions probably sounds terrifying right now, treatment is gradual and done with support. You won’t be thrown into your worst fear on day one. Many people who complete ERP treatment describe it as life-changing, not because the intrusive thoughts disappear entirely, but because they no longer control their lives.
If you recognize these patterns in yourself or a loved one, specialized treatment can make a profound difference. At Take Root Therapy, Lauren Feldman offers evidence-based OCD treatment, with a particular focus on ERP and supporting families through the treatment process. And if we can’t accommodate you, we are glad to help you find suitable resources. You don’t have to struggle alone. Help is available, and recovery is possible.